overview of the spinal ganglion (dorsal root ganglion), covering its anatomy, physiology, biology, histopathology, and clinical significance:
1. Anatomy
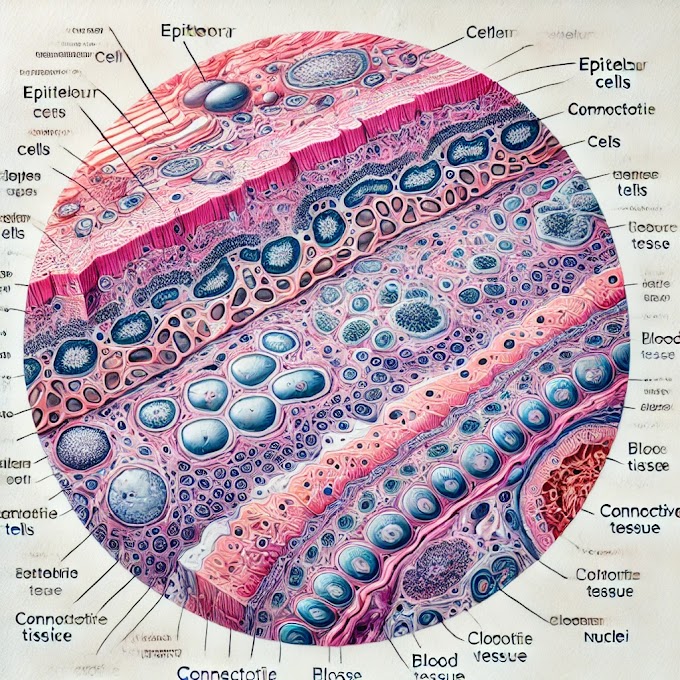
- The spinal ganglion, also known as the dorsal root ganglion (DRG), is a cluster of nerve cell bodies located along the dorsal root of each spinal nerve.
- It contains sensory neurons that transmit signals from peripheral sensory receptors (such as those for touch, pain, and temperature) to the central nervous system (CNS).
- Each sensory neuron within the DRG is a unipolar neuron (or pseudounipolar neuron), with a single axon that branches into two segments: one projecting to the periphery and the other connecting to the spinal cord.
- Surrounding each neuron in the ganglion are satellite glial cells, which provide support and insulation, as well as a connective tissue capsule that protects the structure.
2. Physiology
- The primary function of the spinal ganglion is to act as a relay center for sensory signals. Sensory neurons in the DRG carry information from sensory receptors to the spinal cord, which then transmits it to the brain for processing.
- Unipolar neurons in the DRG allow rapid transmission of sensory signals. The branching structure of these neurons minimizes signal delays, enabling efficient response to sensory stimuli.
- The DRG also plays a role in pain sensation and modulation. It contains nociceptors (pain receptors) that can become sensitized, particularly in response to inflammation or injury, contributing to pain perception.
3. Biology
- Sensory Neurons: The cell bodies in the DRG are responsible for converting physical or chemical stimuli from the periphery into electrical signals that the nervous system can interpret.
- Satellite Glial Cells: These cells surround each sensory neuron and regulate the microenvironment, including maintaining ion balance and modulating signal transmission between neurons.
- Connective Tissue Layers: The ganglion is encased in a capsule of connective tissue, which not only provides structural support but also protects it from mechanical stress.
4. Histopathology
- Inflammation and Degeneration: The spinal ganglion can be affected by inflammatory and degenerative conditions. For example, dorsal root ganglionitis is an inflammation of the ganglion, often associated with viral infections like Herpes zoster (causing shingles).
- Neuropathic Pain: Pathological changes in the DRG, such as neuron hyperactivity, can lead to neuropathic pain, which occurs when nerves are damaged or dysfunctional.
- Trauma: Injury to the dorsal root ganglia, such as from a spinal injury, can result in sensory deficits or chronic pain.
- Tumors: Rarely, tumors such as schwannomas or neurofibromas can form in or near the DRG, leading to pain, sensory loss, or other neurological symptoms.
- Degeneration in Aging: Age-related degeneration in DRG neurons and surrounding tissues may contribute to decreased sensory perception and neuropathic pain in the elderly.
5. Clinical Significance
- Pain Management: The DRG is a significant focus for research and treatment of neuropathic pain because it is where many pain signals are relayed to the CNS. Treatment approaches may include DRG stimulation, a form of neuromodulation that can help reduce chronic pain.
- Herpes Zoster (Shingles): The DRG is a common site for the reactivation of the Varicella-zoster virus, which causes shingles. The virus resides dormant in DRG neurons and, when reactivated, leads to painful rashes and potential postherpetic neuralgia (chronic pain following shingles).
- Diagnostic and Therapeutic Target: Injections and nerve blocks targeting the DRG can be used diagnostically to identify sources of pain or therapeutically to manage chronic pain. Emerging treatments, like DRG stimulation, are being explored for persistent pain relief.
- Spinal Disorders: Conditions affecting the DRG, such as spinal disc herniation or spondylosis, can compress the DRG and result in radicular pain (radiating pain), often seen in conditions like sciatica.
In summary, the spinal ganglion plays a crucial role in sensory signal transmission, pain modulation, and as a target for pain management therapies. Its dysfunction is associated with various sensory and pain-related disorders, making it highly relevant in clinical settings

















0 Comments